The credentialing process validates that a physician meets standards for delivering clinical care, wherein the Payer verifies the physician’s professional profile. Prioritizing credentialing in the RCM process can help avoid challenges such as delay in payor enrolment, billing denials and administrative errors. SHAI provides comprehensive credentialing services

SHAI’s dedicated insurance eligibility verification team delivers a thorough verification, thereby aiding drastic reduction of the clients’ Accounts Receivable cycle.
Prior Authorization offers a significant level of protection for both the patient and the provider. Failing to obtain pre-authorization for a certain procedure or service can jeopardize reimbursement.
Our services ensure patients are approved for procedures before arrival, accurately completing the first stage of the revenue cycle.
We validate and update the following patient information on the practice management system:
We offer industry-leading medical coding services and medical coding audit services, providing high value for every coding dollar you spend on your coding needs. The power of accurate coding becomes instantly visible with drastic reductions in denials and increases in collections.
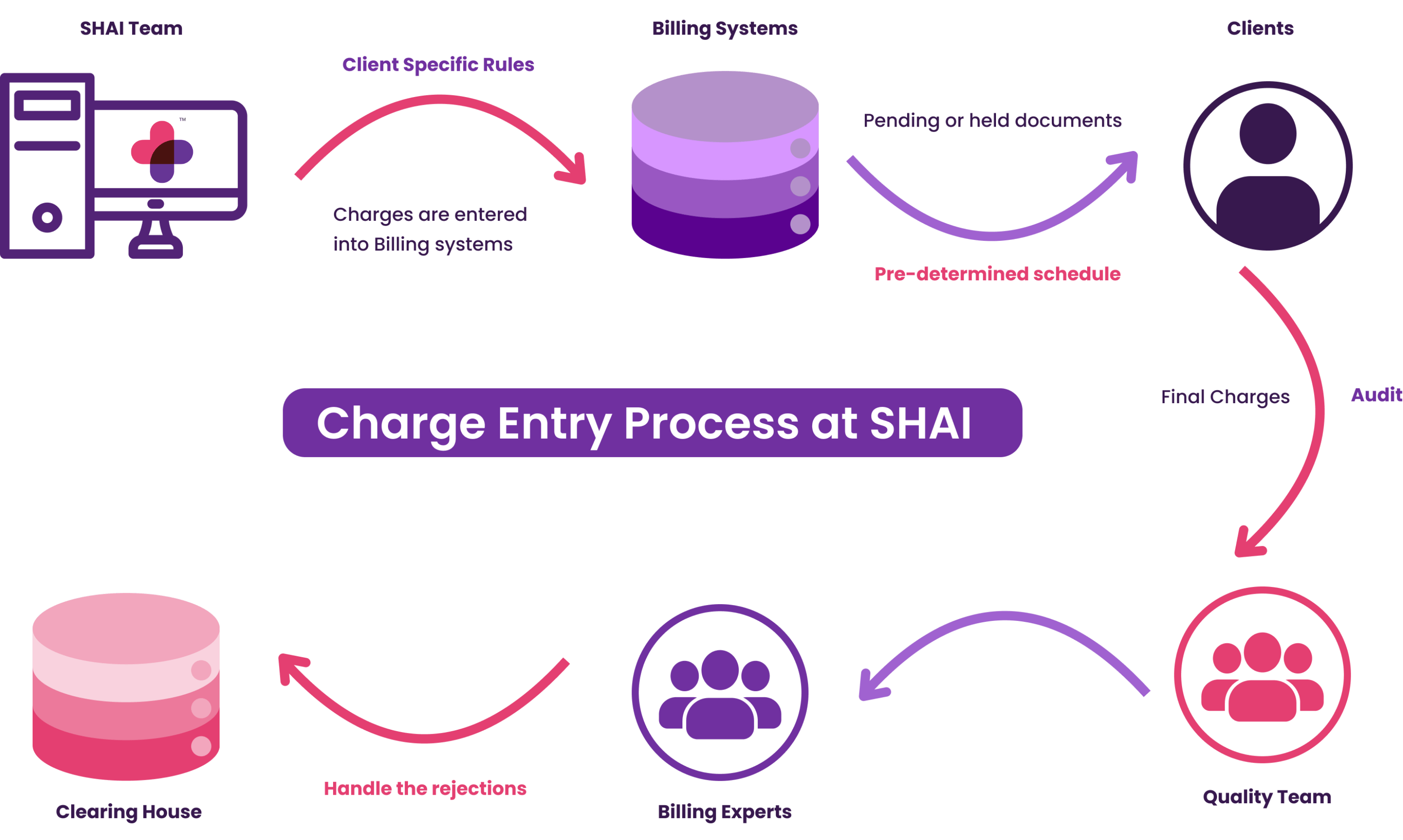
SHAI ensures meticulous attention to detail and prevent any charge entry errors that could lead to claim denials. Additionally, SHAI fosters excellent coordination between the coding and charge entry teams to achieve optimal results.
The accuracy of these charges directly impacts the reimbursements for physicians' services.

SHAI manages the entire process of handling payments for claims. This includes receiving either an EOB (Explanation Of Benefits) or ERA (Electronic Remittance Advice) from payers. SHAI promptly posts these payments into the respective patient accounts to reconcile them against the claims.

Payer correspondence represents a variety of health plan/payer communications. This includes, but not limited to payment denials, explanations, additional documentation requests, authorization approvals, authorization rejections, patient medical necessity determinations and a claim that is under review.
At SHAI, we review the correspondence letter that we receive from the physicians’ office and work them on timely manner. We also work towards preventing any issues that we see in correspondence letters so this does not occur in future.
Credit balance with payers: Providers should process refunds within 60 days from the date of the refund request. We validate each request, and if found to be valid, we process the refund. If the refund request is invalid, we raise an appeal after thorough validation.
The Accounts Receivable (AR) follow-up team in a healthcare organization is responsible for looking after denied claims and reopening them to receive rightful reimbursement from the insurance carriers. Even though these claims could be held up by simple mistakes, you will be surprised to know that over half of the denied or rejected claims are never reworked. This means that the average healthcare provider is leaving thousands of unclaimed dollars on the table every year.
Once the claims get transmitted, we assign an expected payment date against each claim. We closely monitor the payments against the assigned dates. When payments are not received, we do close follow up on the claims to know the status and ensure action is taken if any issues are seen.
In another scenario, it may be possible that not all submitted claims are received by the insurance carrier. One of the biggest delays in payment results from claims not being filed. In simpler terms, the claim wasn’t received by the insurance carrier. This typically occurs when paper claims are lost or misplaced somewhere along the way before they are delivered. To avoid such blunders with paper claims, we allow 10 business days to pass before contacting the insurance firm to confirm whether the claim was received.
Managing denied claims: Depending on the denial reason, we actually send out a new claim request with all required corrections before your practice even receive the paper denial via mail.
We contact the insurance firm and inquire why they denied your claim rather than waiting for the paper denial explaining the reason through the mail, our A/R team can make sure that all claims get corrected as fast as possible.
Resubmitting the claims up to 7 days earlier instead of waiting for the mail will undoubtedly reduce the turnaround time for your payments.
Manage pending claims: At times, claims will be kept pending for a certain duration of time because of additional information needed for the respective member. By executing a proper follow-up, our A/R team can notify the member regarding the situation so appropriate action can be taken and the entire process is sped up again.
We do old AR recovery services for both hospital and physicians. Tracking outstanding accounts receivable and ensuring prompt and timely follow-up with payers to ascertain status
Reports and insights on paid, unpaid and partial paid claims are sent to providers proactively, on a regular basis
Our denial management services handle denial requests and help you analyse the reasoning behind the same and improve the process to bring down the overall denial rate. By understanding the root cause of denials and analysing vital data, your management can take corrective actions that will decrease the rate of denials in the future. This is hence a long-term solution to increase your cash flow and make processes more streamlined and automated.

A patient-friendly statement gets sent to the patient through traditional mailing along with an e-statement on a timely basis. The patient statements by us give clarity about the outstanding and paid amount. Along with it, the patient gets clarity on whom they are paying a particular amount.
Get in touch with us now and Schedule a Call
Book a call